They may look like humble little blocks, but these miracle devices could end animal testing, revolutionize the development of new drugs and lead us into a world of entirely personalized medicine.
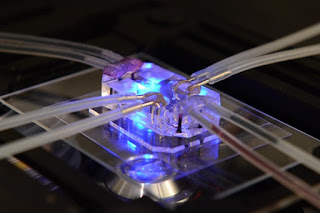
Tiny tubes emerge from a small transparent block, pumping imperceptible amounts of fluid and air to and fro. It looks like a Fox’s Glacier Mint has been plugged into a life support machine, but this humble chunk of see-through silicone is a model organ that could revolutionise the pharmaceutical industry, reducing the need for animal testing and speeding up the development of new drugs.
Meet the Lung-on-a-chip, a simulation of the biological processes inside the human lung, developed by the Wyss Institute for Biologically Inspired Engineering at Harvard University – and now crowned Design of the Year by London’s Design Museum.
Lined with living human cells, the organs-on-chips mimic the tissue structures and mechanical motions of human organs, promising to accelerate drug discovery, decrease development costs and potentially usher in a future of personalized medicine.
The micro-devices work by recreating the tissue interfaces of human organs inside a transparent polymer “chip”, so the behaviours of bacteria, drugs and human white blood cells can be easily monitored through a microscope. A tiny channel runs through the middle, divided along its length by a porous membrane, with human lung cells on one side and blood capillary cells on the other. By running air through one side and a blood-like solution through the other, while applying a flexing and stretching motion using a vacuum, the chip can simulate the processes of breathing.
“The organs-on-chips allow us to see biological mechanisms and behaviors that no one knew existed before,” says Don Ingber, founding director of the Wyss Institute. “We now have a window on the molecular-scale activities going on in human organs, including things that happen in human cells that don’t occur in animals. Most drug companies get completely different results in dogs, cats, mice and humans, but now they will be able to test the specific effects of drugs with greater accuracy and speed.”
Ingber and his team have developed a number of different organs-on-chips to date, including a kidney, liver and peristaltic gut-on-a-chip, while skin-on-a-chip is currently in development for the cosmetics industry and for testing household cleaning products.
The different organs can also be joined up in a network, allowing the journey of a drug to be followed through a simulated human body. The effects of an aerosol drug, of the kind dispensed by an asthma inhaler for example, can be observed in terms of how it enters the lungs, how it affects the heart, how it is metabolized by the liver and how it is excreted by the kidneys, with any adverse side-effects monitored along the way in real time. Four organs have already been tested together for a two-week trial period and in two years’ time, Ingber says they will have 10 organs up and running for a month-long test. So what next? Does this work lead the way to building an artificial human-on-a-chip?